by Marc Andre Jean
The Clarity Times October 6, 2023: Cancer is a devastating disease and ranks among the leading causes of death worldwide, including in the United States. Generally defined as the abnormal proliferation of cells in the body, cancer disrupts the natural cycle of cell growth and death. This uncontrolled cell growth can affect any part of the body, interfering with normal bodily functions. Among the various forms of cancer, pancreatic cancer stands out as a particularly formidable adversary.
Understanding Different Forms of Cancer
Cancer encompasses various types, each named according to the organ or tissue affected. For instance, lung and brain cancers are named after the organs they afflict.
According to the 2019 report by the American Cancer Society titled “Cancer Facts and Figures,” breast, lung, prostate, colon, liver, and pancreatic cancers are among the most common and deadly forms of cancer in the United States. Notably, pancreatic cancer, which accounted for 56,770 new diagnoses and 45,750 deaths in 2019, proves to be a particularly sinister foe.
Overview of Pancreatic Cancer
The pancreas, located behind the stomach, plays a crucial role in bodily functions. It releases essential hormones like insulin and glucagon to regulate blood sugar levels and secretes digestive fluids crucial for food digestion. However, like many organs, the pancreas can fall victim to cancer. When this occurs, it is known as pancreatic cancer.
The pancreas consists of two main types of cells: endocrine and exocrine. Endocrine cells produce hormones such as insulin, which regulate the actions of specific cells and organs. In contrast, exocrine cells generate digestive enzymes released into the small intestine. Pancreatic cancer primarily originates from exocrine cells, accounting for about 95% of cases.
Tracing the History and Causes of Pancreatic Cancer
The history of pancreatic cancer remains shrouded in relative obscurity. Advances in understanding the disease are attributed to figures such as German surgeon Walther Kausch, who performed the first resection of a periampullary cancer in 1909. Another pivotal moment came in 1935 when American surgeon Allen Whipple performed an improved version of the surgery, later known as the Whipple procedure.
The etiology of pancreatic cancer remains elusive, with no definitive cause identified in most cases. However, several risk factors have been recognized, including smoking, family history of pancreatic cancer, genetic predisposition, diabetes, obesity, poor diet, alcohol consumption, and physical inactivity. Exposure to certain chemicals and pesticides in the workplace has also been linked to increased risk.
Understanding the epidemiology of pancreatic cancer is crucial for unraveling its origins and developing preventive strategies. While the precise cause remains enigmatic, studies have pointed to age, sex, and ethnicity as additional risk factors.
Identifying Signs, Symptoms, and Diagnosis
Pancreatic cancer often hides its presence, with symptoms varying from patient to patient. Early detection can be challenging due to the absence of distinct warning signs. Some individuals may only experience vague symptoms easily confused with other abdominal or gastrointestinal conditions. Common indicators include fatigue, depression, abdominal or back pain, jaundice, loss of appetite, nausea, changes in stool color, and recent onset of diabetes.
Late diagnoses are frequent due to these elusive symptoms. To confirm suspicions, doctors use various diagnostic methods, including imaging tests such as ultrasound, CT scans, MRI, and PET scans. These imaging techniques allow for a thorough examination of internal organs, particularly the pancreas.
Blood tests also play a crucial role in diagnosis, helping to evaluate liver function, overall health, and specific tumor markers released by pancreatic cancer cells.
Epidemiology and Global Impact
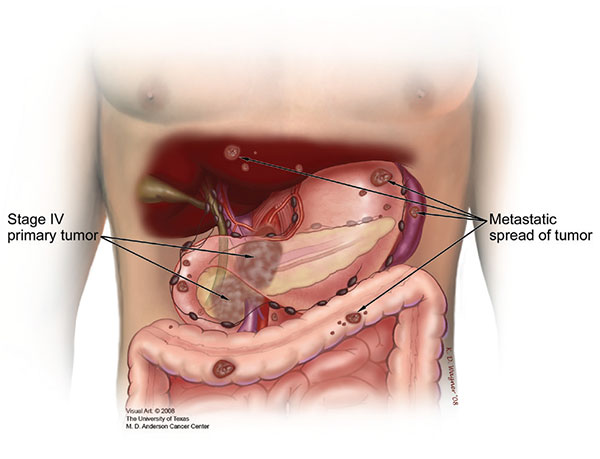
Pancreatic adenocarcinoma is among the most aggressive malignancies worldwide, with a five-year survival rate of less than 5%. Its grim prognosis is due to the lack of reliable early detection methods, its tendency to metastasize early, and its resistance to available treatments. Incidence and mortality rates for pancreatic cancer vary by age, with higher rates observed in older individuals, particularly those over 70 years old.
The highest incidence and mortality rates for pancreatic cancer are found in developed countries such as the United States, Australia, New Zealand, and most European countries.
In 2012, the highest pancreatic cancer incidence rates were in North America, at 7.4 per 100,000 people, and Western Europe, at 7.3 per 100,000 people, followed by other regions of Europe and Australia/New Zealand, with about 6.5 per 100,000 people. The lowest rates, around 1.0 per 100,000 people, were observed in Central Africa and South-Central Asia.
Another aspect of pancreatic cancer incidence rates is related to age. According to Ilic, M. & Ilic, L., incidence rates increase with age for both sexes, with the highest rates in those over 70. Therefore, pancreatic cancer can also be classified as a disease of the elderly, with nearly 90% of all cases diagnosed after the age of 55. Additionally, the same study provides further details on the mortality rate of the disease. The mortality rate for pancreatic cancer varies significantly across different regions of the world.
In 2012, the highest mortality rates due to pancreatic cancer were in North America, at 6.9 per 100,000 people, and Western Europe, at 6.8 per 100,000 people, followed by other European regions and Australia/New Zealand, with a rate of about 6.0 per 100,000 people.
Prognosis, Treatment, and Prevention
Patients with pancreatic cancer face a very bleak prognosis. Unfortunately, the resectability rate for pancreatic cancer remains relatively low. However, even after potentially curative resection, the five-year survival rate ranges from only 15 to 25% in most cases. Although the prognosis is dire, pancreatic cancer can be treated. Treatment depends on various factors such as the stage and location of the disease, as well as the patient’s overall health. Treatment options may include surgery, radiation therapy, chemotherapy, or a combination of these treatments. If the cancer is advanced and surgery, chemotherapy, or radiation therapy are not likely to benefit the patient,
According to the Mayo Clinic, there is no sure way to prevent pancreatic cancer. Some risk factors such as age, sex, race, and family history cannot be controlled, but individuals can reduce their exposure to certain pancreatic cancer risk factors such as smoking, obesity, alcohol consumption, and exposure to certain chemicals in the workplace.
Sources Consulted for This Article:
- American Cancer Society. Cancer Facts & Figures 2013. Atlanta, GA: American Cancer Society; 2013.
- American Cancer Society. Pancreatic Cancer Risk Factors (2019). Atlanta, GA: American Cancer Society; 2019.
- Pancreatic Cancer (2018). Mayo Clinic. Link
- Pancreatic Cancer and the Environment (2016). Link
- Munkley, J. (2019). The Glycosylation Landscape of Pancreatic Cancer (Review). Letters in Oncology, 17(3), 2569+.
- Faisal, M., Fathy, H., Hassan, A., & Elhadry, M. (2019). Effect of Lymph Node Density on the Prognosis of Patients After Pancreatic Cancer Resection. The Egyptian Journal of Surgery, 38(1), 39.
- Howard, J (2002). History of the Pancreas, consulted at [Link]
- Ilic, M., & Ilic, I., (2016). Epidemiology of Pancreatic Cancer
- National Cancer Institute (2015). What Is Cancer?
- Zhang, Q., Zeng, L., Chen, Y., Lian, G., Qian, C., Chen, S., … Huang, K. (2016). Epidemiology, Detection, and Management of Pancreatic Cancer. Gastroenterology Research and Practice
Note: The information provided in this article is for educational purposes only and does not replace medical advice, diagnosis, treatment, or other healthcare services.